What is REDs? The Danger of Energy Deficiency in Female Athletes
By Emily R Pappas, M.S.
Female athletes everywhere know their period will affect how they feel, and how they feel will affect how they perform. Although skipping a few periods or missing a period all together could seem attractive for a female who feels like crap on her period, a missing period or dysfunctional cycle is a HUGE warning sign that cannot be ignored.
This article helps explain what RED-S is, how it affects the female athlete LONG TERM, and what to do if your female athlete exhibits chronic symptoms that include loss or disruption of her period, high rate of injuries, frequent sickness, &/or chronic fatigue. Read on!
In 1972, a short but powerful federal law was passed:
It was an AWESOME win for women in sports. As a result, over the last few decades, our girls’ interest and participation in sports have exploded.
As interest has grown, so has competitiveness.
With scholarships to earn, championships to win, and records to break…things like irregular cycles and missing periods get pushed to the back burner.
After all, getting pregnant is the last thing on the minds of most high school and collegiate athletes…so why does menstrual health matter right now?
The reason is this: hormonal health plays a HUGE role in the overall health and performance of women in sports.
It can affect both performances now…and for the rest of their lives.
Some studies show up to 60% of female athletes experience menstrual irregularities, 30% of which are amenorrhoeic or missing their periods altogether. [2]
Missing periods are a BIG warning sign for a deep, underlying issue that, if left unaddressed, could have disastrous long-term consequences.
We’re talking about Relative Energy Deficiency in Sport (RED-s) and how hormonal health affects not just today’s performance…but long-term success.
Hidden Dangers: Female Athlete Triad And REDs
In the early 90s, sports science research identified the Female Athlete Triad as a syndrome occurring in female athletes involving the interplay of these three things:
Low body fat
Menstrual dysfunction
Poor bone health.
Identifying the problem was the first big step in helping girls become healthy and successful lifelong athletes. Studies showed that if problems were identified and addressed early, most damage was reversible. [2]
But identifying the Female Athlete Triad wasn’t a fix-all.
With this definition, scientists were limited in their understanding of how this syndrome was caused and its effects.
As participation in athletics boomed, more studies began to indicate that female athletes weren’t required to have severely low body fat to suffer from symptoms of the Female Athlete Triad.
Something was happening, and not just to girls. Male athletes were also showing an increased risk of fractures, hormonal disruptions, decreases in performance, and higher long-term risk of poor skeletal health. [3]
So, in 2014, the IOC broadened its statement to address the gaps of previous research, introducing us to an overarching issue called REDs.
In the most updated statement (2018), the IOC produced a consensus statement on REDs relative energy deficiency.
They defined Relative Energy Deficiency in Sports as:
“The impaired physiological functioning caused by relative energy deficiency and includes, but is not limited to, impairments of
Metabolic rate
Menstrual function
Bone health
Immunity
Protein synthesis
Cardiovascular health” [2]
The cause?
LOW ENERGY AVAILABILITY
What Is Low Energy Availability?
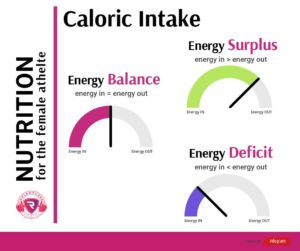
Low energy availability (or LEA) is the driving force behind REDs. It happens when a mismatch exists between an athletes energy intake (her diet) and the energy expended in exercise.
When a female athlete isn’t consuming enough energy to match exertion, the body has trouble finding the energy it needs to support itself as a whole. This causes an athlete to suffer both in short term performance and long term health.
In the lab, we can calculate the LEA by:
[Energy Intake (kcal) – Exercise energy expenditure (kcal)]/ Fat Free Mass (kg)
(Fat Free mass is used to reflect the body’s most metabolically active tissues)
The optimal energy availability is about 45kcal / kg FFM.
When the number nears 30kcal/kg of FFM/day, the athlete runs at a much higher risk of experiencing ailments such as [2]:
Metabolic rate disruption
Menstrual disruption
Loss of bone mass
Cardiovascular issues
Although research shows LEA is the underlying cause of REDs, the methodology of recording intake by self-reports is flawed [4].
This human error makes it difficult to determine exactly when an athlete is in danger and how much more they need to consume to make up for energy loss.
The Unreliable Food Log: Why It’s Not Easy To Determine LEA
Most studies on LEA rely on data collected from athletes in the field.
However, human error makes LEA, and its connection to REDS, very difficult to accurately study.
Most food intake recordings rely on memory and relative measurements. With all of the other immediate concerns our athletes face, it’s no wonder that research indicates most food intake records severely underreport what is actually being consumed [6].
Even more, this number is an APPROXIMATE for the “normal” female athlete.
But what does “normal” mean?
Since opening Relentless Athletics in 2014, I’ve trained hundreds of female athletes. “Normal’ is a bell curve- and athletes lie on different areas of this curve (i.e.: no two athletes are the same)!
Food intake logs are just one diagnostic TOOL that can help us determine if energy availability is low relative to an athlete’s level of energy needs.
More so, food logs can’t always tell us “why” there’s a deficit. Is low food intake an accident…the result of a busy schedule and skipped meals? Or does it represent a larger issue, like a clinical eating disorder?
A Quick Word on Eating Disorders
LEA stemming from true eating disorders is a whole different game.
But how can you tell if an eating disorder is the root cause of underfueling?
When working with coaches and parents on nutrition, here are some red flags I ask they watch for:
High intake of fiber
Use of Stimulants
Artificial sweeteners
Purposely high intake of low energy density foods
High dietary restraint (rules, habits, anxiety surrounding food)
Poor energy levels throughout the day
These habits may be signs of a more serious problem than just not eating enough food on game day. [6]
You may have read this article on how IG model Ruby Matthew’s recently admitted her diet was “a life of tapas and cocaine.”
Obviously, it seems absurd to think the athlete you’re coaching would ever go to such an extreme. However crazy it seems, you have to be aware that these are the social models all women are exposed to everyday.
The girls we parent and coach are constantly bombarded by images defining what is attractive’ and ‘what is accepted’…its not hard to imagine an athlete, trying to compete with social media models, developing a poor relationship with food.
In a study in 2012 performed on Division 1 Female Soccer players, researchers at Penn State noted that 29% of the athletes experienced LEA (< 30kcal/ kg FFM) during the pre- and mid-season. Additionally, these researchers found a strong relationship between those athletes experiencing LEA and those athletes who demonstrate high body dissatisfaction and a high drive for thinness. [7]
When LEA stems from disordered thinking (thanks to misinformation on the media and gurus pushing detox diets and quick fixes), proper nutrition education is key. (more on this in a bit).
However, LEA stemming from true eating disorders requires clinical help.
You - as a parent or a coach - cannot and should not address larger psychological concerns such as obsessive-compulsive, anxiety, and controlling behaviors on your own.
Inadvertent Under-fueling and the Female Athlete
Many female athletes suffer from LEA stemming from inadvertent underconsumption or resulting from disordered eating patterns (not true disorders, but issues generally based on misguided information based on individual experience and not research-based repeatable studies ).
What’s the solution?
Education.
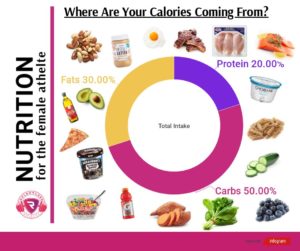
Solving this issue requires education in basic scientific principles of metabolism and sports nutrition.
We aren’t saying go get a PhD, but we are saying that knowledge is POWER in helping athletes
understand the ENERGY DEMANDS their sport has on their body
wrap their heads around the science of how FOOD FUELS their body and helps meet those demands
AND to discuss the misinformation under the context of the social pressures of today.
Instagram “gurus” and models can wreak havoc on real nutritional science.
With nutrition being JUST AS IMPORTANT as training to an athlete, it’s no wonder female athletes struggle more with LEA under the pressures and misinformation of social media.
Raising Lifelong Athletes
REDs and LEA have real, lifelong consequences to our girls.
When your body is severely undernourished, it takes certain steps to CONSERVE energy for more important bodily functions (such as your BRAIN’S ability to function!!). [6]
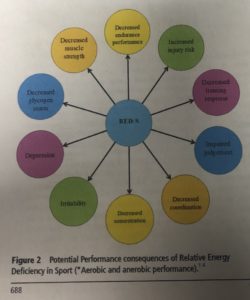
When this happens, REDs becomes a serious syndrome with dangerous long term risks.
The body is a SYSTEM and when one area is affected by low energy availability, other areas reflect this change.
These long term effects include:
alterations to the endocrine system,
poor metabolic function,
disruption of menstrual function,
weakened bone health,
And damage to both cardiovascular and gastrointestinal functions [2]
Here’s what happens to a female athlete suffering from REDs:
ENDOCRINE SYSTEM
In the LEA state, females demonstrate a decrease in Luteinizing Hormone (LH) release from the hypothalamic-pituitary axis, resulting in a decrease in estrogen release in the gonads.
In a healthy female athlete, LH spikes prior to ovulation. With a decrease in LH release and associated hormones that are affected by LH concentration (like estrogen and progesterone) ovulation can become disrupted and even come to a complete halt. [6]
Additionally, a decrease in food availability affects other hormones in the body.
Energy conservation affects thyroid function and changes appetite by affecting the athlete’s regulating hormones (decreased leptin, oxytocin, increased ghrelin, peptide YY, and adiponectin, decreases in insulin and insulin like growth factor, increased growth hormone resistance, and elevations in cortisol levels). [2]
It makes sense.
If the body isn’t getting enough energy, it’s going to conserve what it can for its most vital processes.
MENSTRUAL FUNCTION
LEA plays a role in influencing the hormones that take part in follicular ovulation.
In functional hypothalamic amenorrhea (FHA), a disruption of the gonadotropin-releasing hormone at the hypothalamus causes alterations in LH and FSH release. [6]
This, in turn, causes a decreased estrogen and progesterone levels.
Multiple studies show a direct relationship between the magnitude of the energy deficit and this decrease. [8]
Why is missing or irregular ovulation a problem?
Because during these fluctuations in your hormones, your BONE HEALTH gets hit hard. (more on that in a bit).
Most medical practitioners prescribe oral contraceptives to help reduce irregularity.
But here’s the problem: Oral Contraceptives introduce an exogenous and often synthetic version of estrogen, progesterone (both or just progesterone) to create the hormonal environment that occurs with fertilized egg implantation. The idea is…if your body thinks it is pregnant, it cannot become pregnant. [6]
On the last week of the pill (or the placebo pills), the hormones are removed, telling the body no egg was implanted and it’s time to shed the uterus lining.
Here is the issue:
Introducing an exogenous hormone decreases your body’s own production of that hormone (and those hormones play a part in more than just our sex hormones….men have estrogen too and it’s not because they have ovaries!)
The data regarding the effects of combined oral contraceptives on bone mineral density and fracture risk are INCONSISTENT with most recent studies showing NO or even a DROP in bone mineral density with oral contraceptive use. [2]
Basically, prescribing oral contraceptives treats a symptom- not the root cause.
If a medical practitioner does prescribe oral contraceptives, you must be aware that they might MASK spontaneous menses and bone loss may continue if the energy deficit is not also corrected.
For this reason, the IOC does NOT recommend the use of oral contraceptives for the sole purpose of regulating menses in athletes suffering from RED-S. [2]
BONE HEALTH
Bone health is directly tied to a female athlete’s menstrual health.
When an athlete’s cycle is interrupted (known in the medical community as oligomenorrhea) or completely disappears (amenorrhea), her bone health is at serious risk. These hormonal disruptions cause
Decreases in BONE MINERAL DENSITY
Altered bone microarchitecture
Alterations in bone repair
Decreases in bone strength
Why does this matter?
All of this puts our girls at an INCREASED risk for stress fractures and other bone-related injury. [6]
How? Malnutrition affects more than just energy levels, it also affects micronutrient levels.
For females with REDs, there is a high chance they are NOT getting enough micronutrients for optimal health. Essentially, they aren’t consuming enough to provide for their vitamin D and calcium needs- two micronutrients that are ESSENTIAL to musculoskeletal strength. [2]
A lack of energy, combined with a lack of these essential micronutrients, makes it more difficult for the body to recover from load-bearing activity.
In short: weak bones mean a high risk of injury.
Weak bones in young, developing athletes now can lead to a lifetime of medical issues.
Why?
Bone mass for the female athlete peaks in our 20s. At 26, females have typically reached 99% of their bone mineral content. This isn’t something that can be easily ‘fixed’ down the road. [6]
Reversing the bone mineral loss process is a PRIORITY for adolescent and teen females suffering from RED-S.
The only way to do this is by addressing the low energy availability problem head on through nutritional programs that balance an athlete’s unique level of activity.
CARDIOVASCULAR And GASTROINTESTINAL HEALTH
If hormonal trouble and the risks of lifetime skeletal issues weren’t enough to convince you, LEA also causes damage to both the cardiovascular and gastrointestinal system of the female athlete.
Athlete suffering from LEA have a lowered heart rate and systolic blood pressure. These changes in cardiovascular health increase with the deficit between food vs. output, and can cause valve abnormalities, pericardial effusion, severe bradycardia, hypotension, and arrhythmias. [2]
Gastrointestinal distress is also a common symptom of LEA. As athletes lack enough intake, they can suffer from issues like
Constipation
Delayed gastric emptying
Altered sphincter functions
Stool leakage
It all comes down to putting STRESS on the body.
Lack of energy intake is STRESS.
GI distress is STRESS.
Menstrual disturbances are STRESS.
CV alterations are STRESS.
All this stress without recovery is detrimental to the athlete. It increases her risk of injury and illness.
Of course, in a high-stress environment, the chances of optimal recovery are slim. This not only causes a performance decrease in today’s game…but next season, too.
LEA: How Under-fueling Undermines Performance
Lower energy availability.
Hormonal imbalances.
Weakened bone structure.
Compromised cardiovascular and gastrointestinal health.
When an athlete is working with a sub-optimal system, her performance will also suffer.
Food is the fuel that provides the energy you need for high bursts of activity. In the short term, LEA affects the amount of fuel available to muscles to perform at the very moment we need them the most.
Over the course of a season, LEA affects an athlete’s ability to recover.
Replenishment of glycogen stores and protein synthesis is impeded without proper supply of energy. This has a HUGE negative impact on an athlete’s physical, mental, and psychological capacity to handle the high intensity challenges of her sport.
Addressing RED-S Head On
Relative Energy Deficiency is a SERIOUS problem in female athletics…with some SERIOUS long term consequences.
In a world guided by social media “realities”, there is a high emphasis on appearance and pressure for “thinness” placed on our athletes.
For adolescents exhibiting LEA, there are at a corresponding higher risk of depression, psychosomatic disorders, and have more trouble managing stress.
Our job as coaches and parents is to EDUCATE our athletes to help proactively address the risks of under-fueling.
For younger female athletes, knowledge is KEY to helping them perceive food as FUEL and not something associated as “good” or “bad” for their bodies. We must teach them the NEEDS of their body and how these affect their ability to perform and recover.
Giving young female athletes a foundational understanding of nutrition helps them develop a positive relationship with how they fuel as their level of performance increases.
If your athlete is already exhibiting symptoms like
loss or disruption of menstruation
high rate of soft tissue or bone injuries
frequent sickness
chronic fatigue
Or showing a disordered relationship with food: (detox diets, cleanses, purposefully high intake of fiber, overuse of stimulants, or a high anxiety around food), the time to act is NOW. Parents and coaches, don’t be afraid to seek help from a nutrition coach or an expert in the field.
After all, the life of a young athlete is stressful. You’re already helping them develop a love of sports through physical training, teamwork, and coaching - nutrition education is just another key part of helping them succeed for life!
REFERENCES
[1] https://www.womenssportsfoundation.org/advocate/title-ix-issues/
[2] Korsten-Reck, U. (2016, 03). The IOC Consensus Statement: Beyond the Female Athlete Triad – Relative Energy Deficiency in Sports (RED-S). Deutsche Zeitschrift Für Sportmedizin, 2016(03), 68-71. doi:10.5960/dzsm.2016.222
[3] https://blogs.bmj.com/bjsm/2017/04/04/optimal-health-including-male-athletes-part-2-relative-energy-deficiency-sports/
[4] Donaldson, S.I. & Grant-Vallone, E.J. Journal of Business and Psychology (2002) 17: 245. https://doi.org/10.1023/A:1019637632584
[5] Stone, A. A. (2000). The science of self-report: Implications for research and practice. Lawrence Erlbaum Associates.
[6] THE YOUNG FEMALE ATHLETE. (2018). SPRINGER.
[7] Reed, J. L., Souza, M. J., & Williams, N. I. (2013, 02). Changes in energy availability across the season in Division I female soccer players. Journal of Sports Sciences, 31(3), 314-324. doi:10.1080/02640414.2012.733019
[8] Loucks, A. B. (n.d.). Influence of Energy Availability on Luteinizing Hormone Pulsatility and Menstrual Cyclicity. The Endocrine System in Sports and Exercise, 232-249. doi:10.1002/9780470757826.ch18